Kenyan Women Embrace IUDs, But Pain Management Remains a Challenge
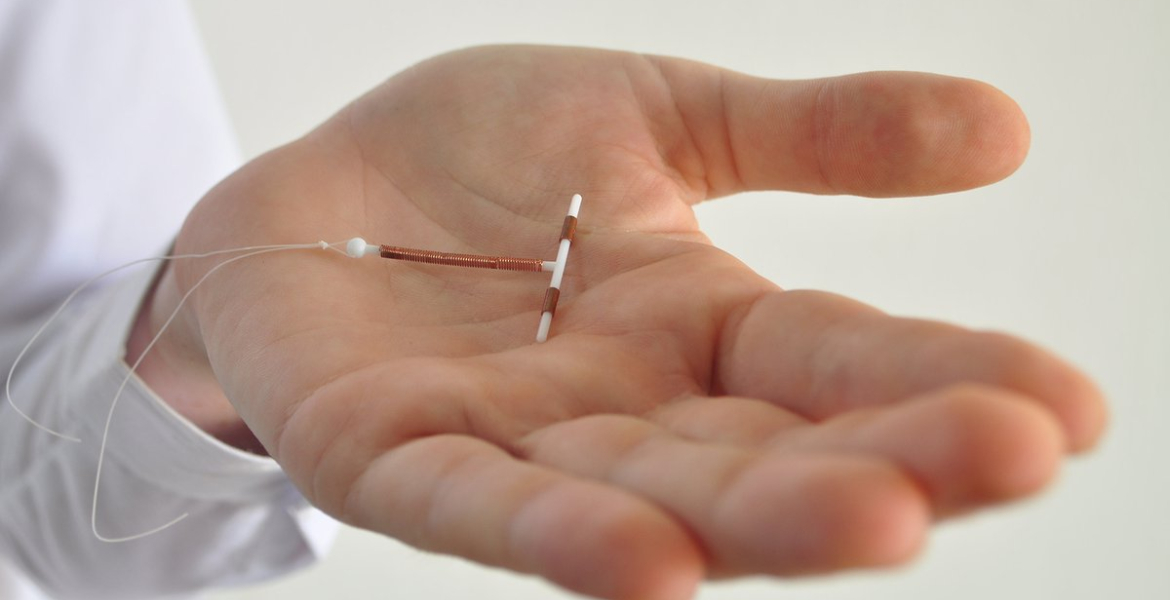
Intrauterine devices (IUDs) are gaining traction among Kenyan women seeking long-term contraception, yet lingering concerns about pain during insertion threaten to undermine this progress.
Recent data indicates a rising adoption rate, underscoring the need for enhanced pain management protocols to ensure comfort and informed consent. The Kenya National Bureau of Statistics reports that 77,126 women opted for IUD insertions last year, marking an increase from 73,457 the previous year. This upward trend is attributed to improved access to reproductive healthcare services and a growing preference for long-term contraceptive solutions among women.
However, alongside this increase is the ongoing challenge of managing pain during the IUD insertion process. While some women experience mild cramping, others report intense, sharp pain akin to severe menstrual cramps. Dr. Vincent Nyangweso of Goldin Medicare explains, "The experience varies widely. Factors like vaginal childbirth history or a naturally tight cervix can significantly influence pain levels."
The insertion procedure involves stabilising the cervix, measuring the uterus, and positioning the IUD within the uterine cavity. Although the entire process typically lasts between 90 seconds and three minutes, the pain experienced during these steps can be substantial, particularly for first-time patients. Dr. Nyangweso also notes that some women may experience dizziness or nausea due to a vasovagal response triggered by cervical manipulation.
Women with a history of trauma related to pelvic examinations may also have heightened sensitivity, intensifying their discomfort. Despite these known challenges, many healthcare providers in Kenya lack standardised pain management protocols for IUD insertions.
The medical community is now being urged to prioritise women's concerns by implementing comprehensive pain relief strategies before, during, and after the IUD insertion. Studies suggest that healthcare providers often underestimate the discomfort, leaving patients unprepared for the potential pain.
The American College of Obstetricians and Gynaecologists (ACOG) has issued updated guidelines emphasising patient-centred approaches. These guidelines advocate for clear communication, realistic expectation setting, and thorough informed consent.
"Women deserve accurate information about the procedure and how pain can be effectively managed," ACOG states.
To minimise discomfort, clinicians are advised to develop personalised pain relief plans based on individual risk factors. These plans may include oral medications, such as ibuprofen or naproxen, taken in advance to reduce inflammation. Additionally, local anaesthetics such as lidocaine sprays, creams, or paracervical blocks can numb the cervix and reduce insertion pain.
The guidelines also highlight the need for trauma-informed care, especially for patients with histories of abuse or medical anxiety. Healthcare professionals should be trained to recognise signs of distress, such as pale skin and dilated pupils and adjust their approach accordingly. A compassionate, empathetic environment can significantly improve patient experiences. Traditional directive counselling is also being reconsidered in favour of collaborative decision-making.
"Patients should feel empowered, not pressured, when choosing a contraceptive method," Dr. Nyangweso emphasises. "It's not just about inserting an IUD but providing holistic reproductive care."
Misinformation remains a significant barrier to informed decision-making. Some women mistakenly believe that IUDs can only be inserted during menstruation or that cervical cancer screenings must precede the procedure. Dispelling these myths and offering clear explanations ensures that women make decisions based on facts, not misconceptions.








Add new comment